Case Presentation
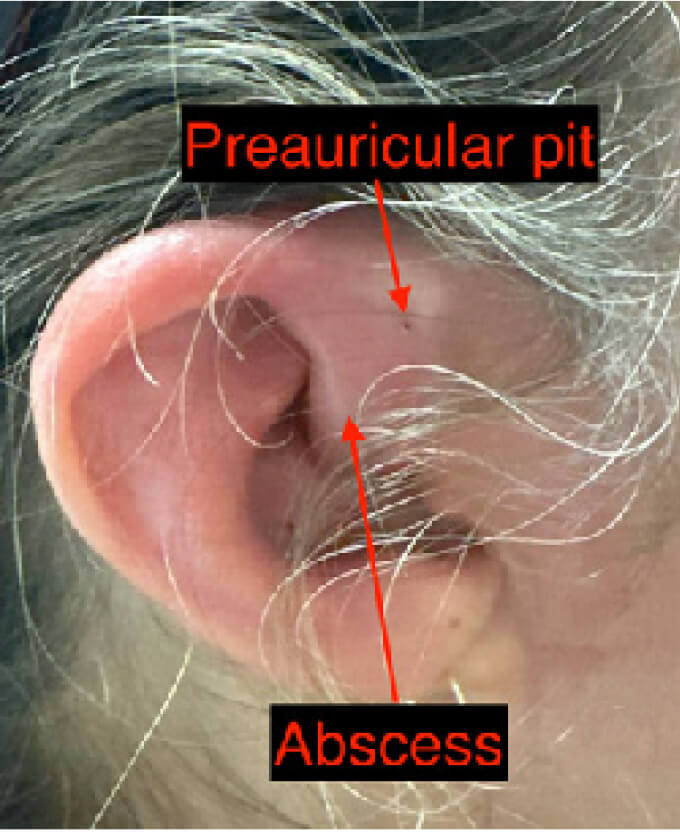
A 50-year-old female with a past medical history of a right preauricular sinus tract, previously complicated by abscess requiring aspiration presented to a community Emergency Department (ED) with four days of worsening right ear pain associated with chills. She had initially been evaluated on day one of symptoms at an urgent care and was prescribed ciprofloxacin without improvement. This was followed by the addition of cephalexin at a second visit, however her pain significantly worsened and therefore presented to the ED for a third visit.
On exam, there was moderate swelling, erythema and warmth of the superior aspect of the right helix and crus of the helix, with induration superior to the tragus (Figure 1). Examination for fluctuance was limited due to significant hyperesthesia of the area. A point-of-care ultrasound was performed with a high-frequency linear probe with a copious amount of gel to prevent any additional pressure to the area. The ultrasound demonstrated a 1.8cm x 0.8cm x 0.7cm anechoic collection just superior to the tragus (Figure 2). We identified an optimal point of needle entry after visualizing surrounding vasculature on color doppler (Figure 3). An 18g needle was used to perform an aspiration and drainage, which removed 1cc of purulent material with significant improvement in pain. The patient was treated with vancomycin and piperacillin/ tazobactam and was admitted for IV antibiotics and observation. Ultimately, a wound culture resulted as Enterococcus faecalis infection and the patient was successfully discharged with oral antibiotics.