Program MAPP to CU is a pipeline program developed in New York City in 2021. This article highlights its utility as both an educational initiative and a Social Emergency Medicine initiative.
EDUCATION
New York American College of Emergency Physicians
Mentoring for Success in Medicine: A New York City Pipeline Program
Disparities in educational and mentorship opportunities for students of color and students from disadvantaged backgrounds are a major contributing factor to under representation of people from underserved backgrounds in medical school enrollment and the physician workforce. This under representation significantly negatively impacts the educational experience of all medical students1 and the healthcare of patients from these populations. When cared for by physicians who have similar backgrounds, patients from underrepresented populations have improved access to healthcare, higher satisfaction with their healthcare and increased acceptance of preventative services.2-5
Despite the critical importance of increasing the proportions of students and physicians from underrepresented populations, the number of medical school applicants from these populations remains alarmingly low. Data from the Association of American Medical Colleges for 2023-2024 shows that of 52,577 medical school applicants, only 4,672 identified as Black/African American and 3,177 as Hispanic/Latino. Of the students who began their first year of medical school in 2023, 1,493 (12.7% of matriculants) identified as Hispanic/Latino, a slight increase compared to the previous year. However, the number of students who identified as Black/African American decreased to 1,845 (10% of matriculants).6
How can we address this underrepresentation in medical schools? A solution lies in reaching out to students early on in their educational experience and ensuring the pool of medical school and other healthcare professional school candidates is large enough to adequately represent and serve patients from disadvantaged populations. Pipeline programs are instrumental in this effort. They serve to spark interest in medicine from an early age and guide young people in achieving future success in a healthcare career. This premise underlies the Mentorship and Pipeline Program at Columbia University (MAPP to CU) founded in 2021 by the Columbia University Irving Medical Center (CUIMC) Department of Emergency Medicine Social Emergency Medicine Committee.
Research suggests that mentorship programs in healthcare can be effective in increasing high school students’ interest in healthcare professions.7,8 These programs often involve pairing students with medical professionals for mentoring, job shadowing and interactive sessions.9,10 They can be particularly beneficial to students from underrepresented backgrounds. Follow-up studies have demonstrated that participants in these programs are more likely to remain committed to healthcare careers and pursue relevant post-secondary education.7,10 Early exposure through volunteering and shadowing opportunities has also been associated with increased interest in medical education and positive adolescent development.11 Overall, mentorship programs appear to be a promising strategy for encouraging high school students to consider and pursue healthcare careers.
Mentorship programs like MAPP to CU have been established throughout the country at other academic institutions. Hospital-based multidisciplinary mentoring initiatives have demonstrated positive impacts on students’ decisions to pursue healthcare careers, with high rates of enrollment in health science degree and pre-medical programs.12 These mentorship initiatives offer hands-on activities, networking events and career panel discussions to help students better develop an understanding of the healthcare professions. 9 Such initiatives not only promote diversity in healthcare but also contribute to creating a workforce that better reflects and serves diverse communities.9,11

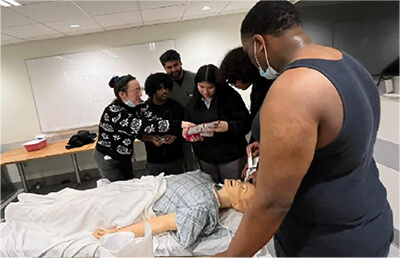
MAPP to CU is a two-year longitudinal pipeline program that partners the CUIMC Department of Emergency Medicine with local high schools. Students from these high schools attend monthly workshops at the medical center campus. Emergency Medicine faculty and trainees and other healthcare providers mentor these students and teach practical healthcare-related skills. Participating high school students represent and reflect the communities served by CUIMC and many are from households where English is not the first language.
Topics covered during the skills-based MAPP to CU workshops include chest compressions, airway management, Stop the Bleed skills, suturing, splinting and bedside ultrasound. These workshops were designed to provide both background education and hands-on experience to pique interest in healthcare. Students learn vital signs, CPR and tourniquet skills that may someday prove crucial and lifesaving within their communities. Also, through these workshops, students are exposed to variety of healthcare professions such as pre-hospital care, nursing, pharmacy, social work and physical therapy.
During their second year in MAPP to CU, students further explore careers in medicine and healthcare with professionals from other specialties including surgery and pediatrics. Students participate in more advanced activities such as a toxicology walk and a comprehensive simulation incorporating skills learned in the first year. Additionally, second-year students are mentored one-on-one in conducting research on a medical or healthcare topic of interest and presenting their findings to their peers. This activity provides students with experience in the process of formulating and answering a research question and communicating their findings. It also promotes self-efficacy and intellectual curiosity.
For high school students, participation in extracurricular activities increases their success in the college application process and facilitates self-discovery. However, for students from lower-income households, afterschool activities often compete with jobs students may need to contribute income to their households. To help address financial barriers that may prevent students from participating in MAPP to CU, students are given gift cards based on their attendance.
MAPP to CU recently completed its third year and celebrated its first class of alumni returning for the second class’s graduation. Thus far, we have noticed students becoming increasingly more confident as they progressed through the program. Many students began the program needing translation services because English was not their first language. At the end of the two-year cycle, many were able to present independently in English their research on complex medical and healthcare topics. Additionally, with increased confidence levels, these students have aspired to goals that may have previously seemed unrealistic or impossible. With the most recent class of MAPP to CU graduates, several students developed plans to pursue careers in nursing and surgery because of their participation in MAPP to CU. The long-term impact of this pipeline program on the participating students and their communities is still unfolding. We are optimistic that students will remain engaged and continue their paths towards careers in medicine and healthcare with MAPP to CU supporting them.
In summary, like other pipeline programs, MAPP to CU aims to address the educational and mentorship needs of students from racial, economic and social backgrounds historically underrepresented in medicine and improve the representation of these students in medical student enrollment and the physician workforce. More specifically, MAPP to CU focuses on students from the population the CUIMC Emergency Department serves. When developed, the overarching goals of MAPP to CU were to provide underrepresented students with opportunities they would not have had otherwise and to increase diversity in the healthcare workforce by exposing these students to healthcare careers and supporting them in their healthcare career aspirations. With the successful graduation of two MAPP to CU classes, we believe we are well on our way to achieving these goals.
References
- Whitla D, Orfield G, Silen W, et al. Educational benefits of diversity in medical school: a survey of students. Acad Med. 2003;78(5):460-6.
- Saha S, Komaromy M, Koepsell T, et al. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159(9):997-1004.
- Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43(3):296- 306.
- Cooper LA, Powe N. Disparities in patient experiences, health care processes, and outcomes: the role of patient–provider racial, ethnic, and language concordance. Commonwealth Fund 2004.
- Alsan M, Garrick O, Graziani G. Does diversity matter for health? experimental evidence from Oakland. Am Econ Review. 2019;109(12):4071-4111.
- . FACTS: applicants, matriculants, enrollment, graduates, MD-PhD, and residency applicants data. December 12, 2023. Accessed July 15, 2024. https://www.aamc.org/data-reports/students-residents/report/facts
- Cervantes L, Chu E, Nogar C, et al. A Hospitalist mentoring program to sustain interest in healthcare careers in under-represented minority undergraduates. J Hosp Med. 2014 Sep;9(9):586-9.
- Robinson M, Douglas-Vail M, Bryce J, et al. Medical school outreach and mentorship for rural secondary school students: a pilot of the Southwestern Ontario Medical Mentorship Program. Can J Rural Med. 2017 Spring;22(2):62-67.
- Shaw K, Schmidt C, Richards-May K, et al. Abstract 13914: Development of a high school mentorship and scholarship program to promote interest in healthcare among students underrepresented in medicine. Circulation. 2023;148(Suppl 1).
- Patel S, Rodriguez P, Gonzales R. The implementation of an innovative high school mentoring program designed to enhance diversity and provide a pathway for future careers in healthcare related fields. J Racial Ethn Health Disparities. 2015 Sep;2(3):395-402.
- Muncan B, Majumder N, Tudose N. From high school to hospital: how early exposure to healthcare affects adolescent career ideas. Int Journal of Med Educ. 2016;7:370–371.
- Danner O, Lokko C, Mobley F, et.al. Hospital-based, multidisciplinary, youth mentoring and medical exposure program positively influences and reinforces health care career choice: the reach one each one program early experience. Am J Surg. 2017;213(4):611-616.