Case Presentation
A 22 year old G1P0010 female presented to the Emergency Department (ED) with vaginal bleeding and an episode of syncope. She started bleeding ten days ago after receiving mifepristone for a missed abortion (estimated gestational age of 10 weeks and 6 days). She continued to bleed intermittently so she was also given misoprostol. On the day of her ED visit, she syncopized while in the bathtub and was still having vaginal bleeding despite the misoprostol.
Upon her arrival to the ED, her initial vitals were: blood pressure of 84/43, heart rate of 172, respiratory rate of 25, with an oxygen saturation of 97% on room air, and a temperature of 38.2 C. On physical exam, she was disoriented and appeared pale and diaphoretic. She was also noted to have active vaginal bleeding with golf-ball sized clots. The differential of her hypotension included hemorrhagic shock versus septic shock from possible retained products of conception (RPOC).
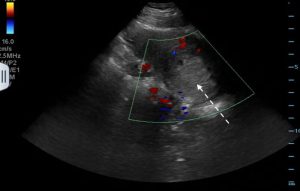
Point-of-care ultrasound was performed and revealed a hyperechoic, heterogeneous mass in the uterus with a thickened endometrial stripe, concerning for RPOC (Figure 1). There was no free fluid visualized and the endometrium was not hypervascular on color Doppler (Figure 2). Obstetrics Gynecology (OB Gyn) was consulted for definitive management. The patient was treated with empiric antibiotics and was given intravenous fluids as well as blood products. She was emergently taken to the operating room (OR) with OB Gyn for a dilation & curettage (D&C). The surgical specimen sent from the D&C showed decidua and immature placenta, confirming the diagnosis of RPOC.