Case Presentation
A 17-year-old male with no significant past medical history presented to the emergency department after being a restrained driver in a motor vehicle accident. Airbags deployed, the patient was restrained, denied loss of consciousness and had full recollection of the events. The patient reported wrist pain and believes they jammed their outstretched wrists into the steering wheel or dashboard.
Physical examination revealed a superficial friction burn over the right anatomical snuffbox with tenderness to palpation in the same area and pain with axial loading of the right thumb. No snuffbox tenderness was noted in the left wrist. The patient’s vital signs were stable.
A X-ray of the right wrist showed no acute fracture or dislocation, growth plates are fused (Figure 1A).
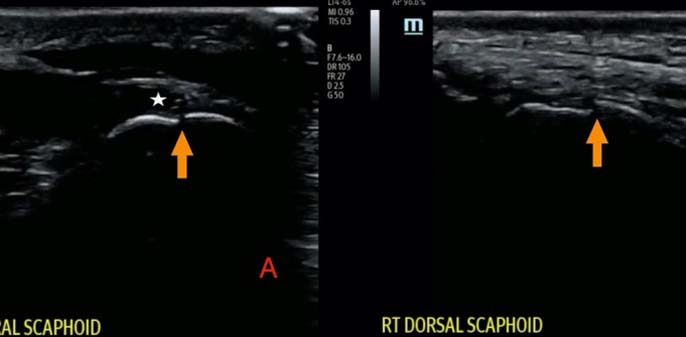
Point-of-care ultrasound (POCUS) of the wrist was performed with a L14-6s linear transducer (Mindray Te7, Mahwah, NJ, Shenzhen, China) that demonstrated cortical discontinuity along the dorsal and volar aspects of the scaphoid bone, concerning for radiographically silent scaphoid fracture, consistent with exam (Figures 2A and 2B).
The patient had minor burn care and was splinted in a thumb spica in a neutral position and was given an orthopedic referral and followed up seven days later with repeat X-rays. Repeat assessment in the orthopedic office one week later demonstrated continued snuffbox tenderness. The repeat X-ray (Figure 1B) revealed a fracture in the proximal third of the scaphoid that was identified by POCUS during the initial Emergency Department (ED) visit one week prior.