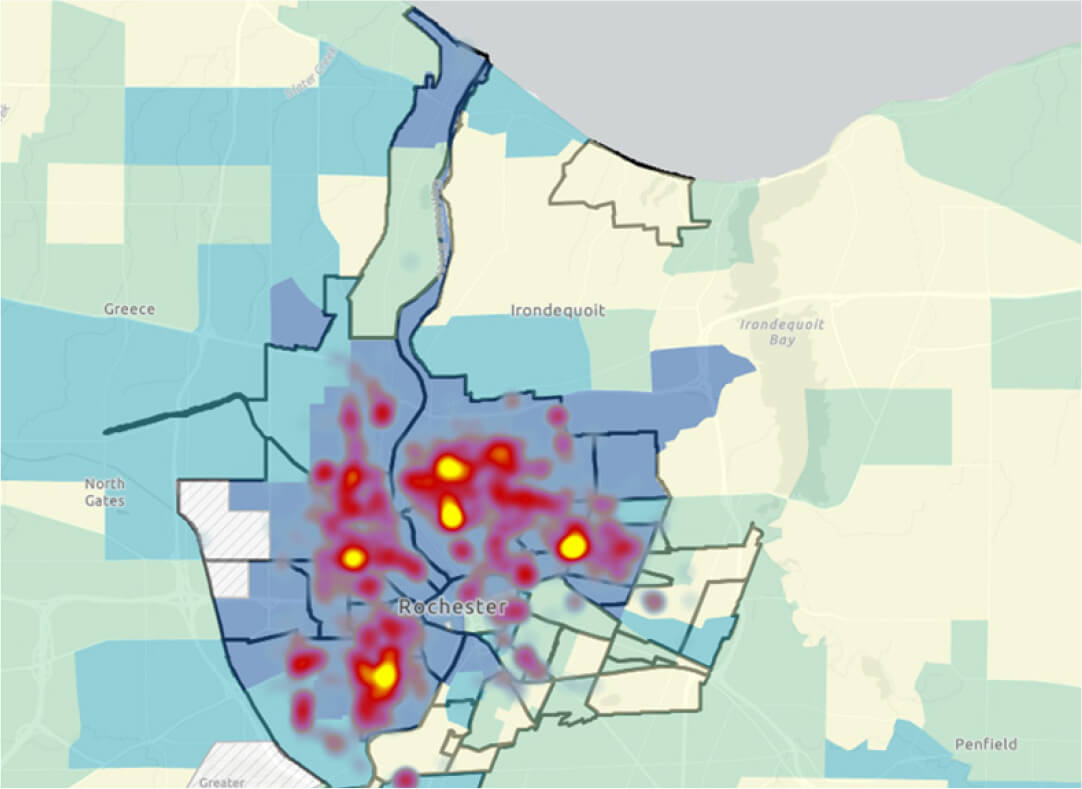
Geospatial techniques lend themselves well to readily understandable presentations of data, such as “heat mapping.” An example of a heat map of publicly available data from the city of Rochester on shooting victims7
(Figure 3) demonstrates how these data sets can quickly be transformed into researchable information on topics germane to the ED. When combined with the data available from an ED EHR, one can easily start to see the power of these techniques to show important associations between health outcomes and public policy issues. The breadth of data relevant to the ED that can be represented in this way is immense, encompassing such differing topics as access to care, social determinants of health, acute injuries and trauma, successful (or unsuccessful) management of chronic medical diseases, etc.. Heat maps are easily interpretable by the general public and policymakers, which helps physicians to direct policy and resources at a state and national level. The power of this kind of representation in advocacy should not be understated.
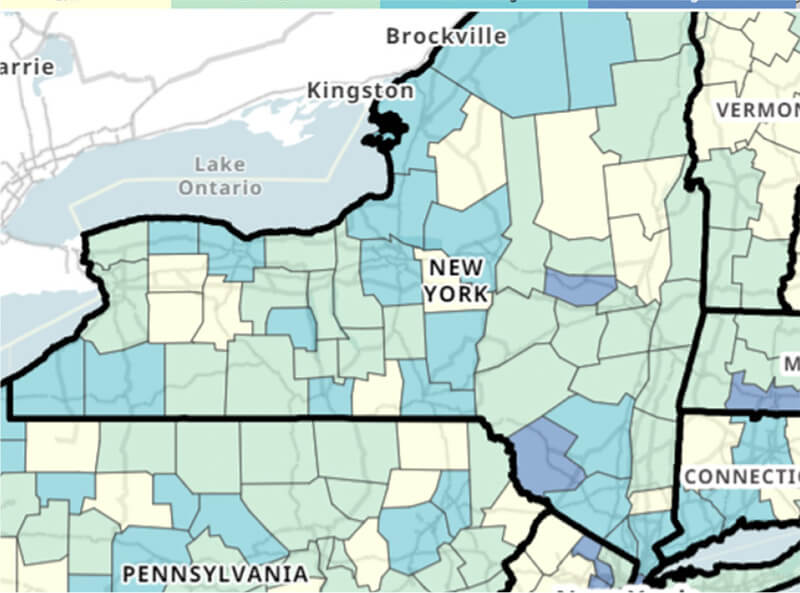
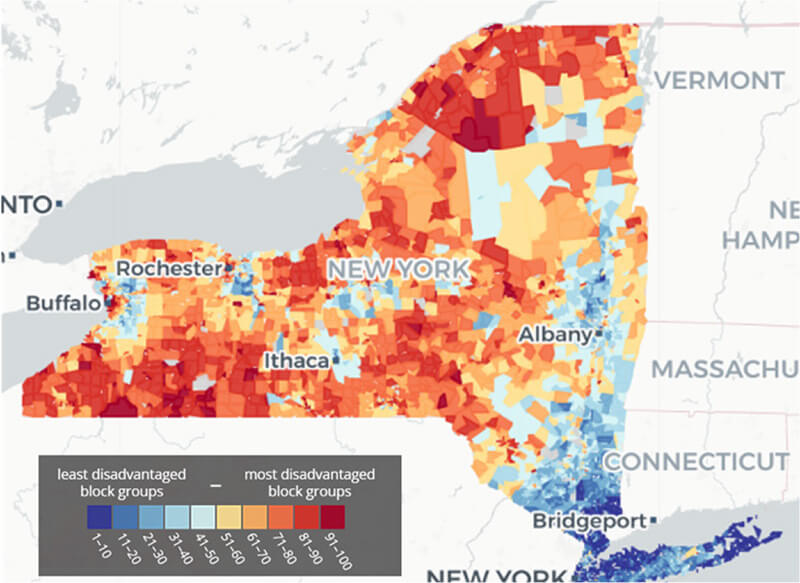
A local example of recent geospatial-driven research from our institution focuses on mapping out-of-hospital cardiac arrest (OHCA) to identify areas of higher community vulnerability. Using a combination of the techniques described above, the researchers were able to demonstrate associations between OHCA and communities with significantly higher SVI and ADI metrics. This kind of data mapping would, in theory, allow EMS agencies to distribute resources according to the frequency of cardiac arrests in the areas they cover. Furthermore, on a larger scale, state and local agencies can begin to address the underlying socioeconomic causes that are correlated with the increase in morbidity of these geographic areas, thus providing an opportunity to further assess health disparities on the basis of neighborhood.
Geospatial driven research holds additional potential in the current climate of massive volumes and overcrowding in EDs across the country. While the ED is, in many respects, a “laboratory of public health,”8 there are significant limitations to how much the ED can provide when its spatial and human resources for the critically ill patients it was designed to manage are stretched thin. Outside of emergency care, managing how best to apply resources to the public, both in the department and in the community, is paramount. Geospatial mapping identifying neighborhoods with frequent low-acuity visits, for example, could direct the placement of an accessible walk-in clinic or urgent care. This results in multiple benefits, including diverting flows of people with lesser acuity away from EDs, decompressing waiting rooms and potentially freeing up both hospital resources and EMS transportation for patients with higher acuity needs. This is a basic example of the application of geospatial techniques to guide upstream changes in patient flow as well as management of ED resources, but the possibilities of geospatial-driven research in this area are numerous.
Much as Emergency Medicine is uniquely poised to respond to acute illness, it also possesses unique data that, with the new tools of geospatial research methodologies and software, can lead efforts in prevention. By projecting real world outcomes data from the ED out into the community through geospatial techniques, we can begin to look for correlations among the changes at play in policy, environment and society, with actual concrete outcomes data. Geospatial-driven research initiatives hold the potential to be an effective means of improving clinical outcomes, guiding preventative medicine and mitigating upstream contributors to the disease processes that bring people to the ED. If these research tools are applied well, we can hope to reduce ED utilization and overall disease burden in our communities.