
17 Jan The MATTERS Team

The MATTERS team
Interviewees:
Joshua Lynch, DO FACEP
Associate Professor of Emergency & Addiction Medicine
University at Buffalo & Chief Medical Officer, MATTERS
Lucy Connery, MPH
Marketing Coordinator, MATTERS
Interviewers:

Sophia Lin, MD FPD-AEMUS
Assistant Professor of Clinical Emergency Medicine and Clinical Pediatrics
Director of Emergency Ultrasound
Department of Emergency Medicine
Weill Cornell Medicine

Joshua Schiller, MD
Director of Global Health/Social Emergency Medicine
Attending Physician
Maimonides Medical Center
Can you tell us about the MATTERS program, and how it is relevant to EM practice?
MATTERS was developed to serve as a “one-stop” solution to linking people with opioid use disorder (OUD) out of the emergency department. We efficiently connect individuals with OUD to an outpatient treatment organization of their choice through our rapid referral platform. Patients choose from over 2,500 weekly appointment slots that are offered by over 250 unique treatment organizations and can choose to follow up in-person, virtually, or in a hybrid model. Individuals are also provided with several barrier-reducing resources and services at their time of referral to ease the minds of emergency medicine (EM) providers when sending patients for follow-up treatment. EM providers can submit referrals in as little as three minutes, and we’ve ensured that the process is efficient and intuitive so that it doesn’t impose any unnecessary burden on their existing workflows. This program is especially relevant to EM practice as emergency departments (ED) are typically the ‘first line of defense’ for individuals with OUD who present in acute withdrawal/post-overdose. If this process can work in large tertiary care centers along with small critical access hospitals, it can work almost anywhere.
How is MATTERS able to provide for your patient communities?
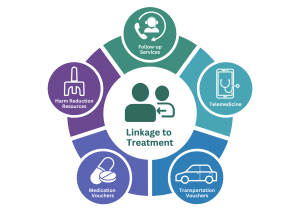
We’ve expanded our platform and services through a patient-centered approach by listening to feedback from patients and network partners. Patients choose where they want to follow up based on their geographic location, preferred treatment model (virtual, in-person, hybrid), and other services offered by each participating treatment organization. These treatment centers will accept any patient regardless of insurance status, polysubstance use, and previous treatment history. As part of the referral process, the MATTERS medication voucher is automatically issued to uninsured and underinsured individuals to cover the cost of up to 14 days of any combination buprenorphine/naloxone prescription that is issued at the time of referral – and we recommend this “bridge prescription” in our standardized protocol to ensure patients have flexibility when they’re following up to care. MATTERS also automatically provides a free, round-trip ride to patients who need it for their first follow-up appointment, no questions asked. Everyone referred through our program can opt-in to be contacted by a peer in recovery, offering an extra layer of support during the earlier stages of their recovery. Our staff also follows up with everyone within 72 hours of their referral to help navigate barriers to treatment and link patients to the support services they need to succeed. We then follow up again at 30, 60, and 90 days to ensure continuity of care.
ALL OF THIS is completed in as little as three minutes. Individuals who are not linked to care can visit our website and get evaluated for substance use disorder through our telemedicine services. In as little as an hour, people are connected via video with a prescriber, where they can receive a prescription for medications for OUD (MOUD) and receive a MATTERS referral with all of the wrap-around services we offer. This reduces barriers to treatment for many people with significant transportation barriers.
We also understand that not all patients are ready for treatment. For people who are unsure about seeking treatment, we distribute free harm reduction supplies to anyone across our networks. This not only helps prevent the risk of overdose, but also creates a relationship with people who use drugs so that if/when they are ready for treatment, they know we are here to help.
Are there certain demographics that are particularly affected by this programming?
For the first time in nearly a decade, national rates of opioid overdose deaths decreased in the U.S.; however, this is mainly applicable to Non-Hispanic White populations. Black, Indigenous, and People of Color (BIPOC) communities are affected by opioid and substance use disorders at a disproportionately higher rate compared to their white counterparts. We also know that people experiencing homelessness are disproportionately affected by substance use disorder due to the unique challenges they face. This calls for services to provide barrier-reducing support to engage marginalized communities.
We also know that there are inequities in the kinds of MOUD these communities receive. Unfortunately, Black and Brown communities are much less likely to be prescribed buprenorphine when compared to White individuals. There are various reasons for this, but the leading “cause” is racial bias and systemic discrimination. We focus on expanding access to buprenorphine across all communities through standardizing prescribing protocols for physicians new to providing MOUD treatment.
How did the development of MATTERS come about?
After years of working in the emergency department, there was a common theme: people with OUD were repeatedly coming back to the ED for treatment. We thought to ourselves: what isn’t working? When we asked the patients this question, we often heard that they were discharged with a long list of phone numbers to call and schedule a follow-up appointment for treatment. When patients tried to call these numbers, they were either out of service or an appointment wasn’t available for weeks at a time. This led to patients feeling like they were at yet another dead-end when seeking treatment and resulted in them returning to the ED.
The fact of the matter is that the experience would be much different if the patient presented with a cardiac concern. Those patients are immediately prescribed medication and receive a follow-up appointment before they leave the hospital. When we asked treatment organizations, they were eager to accept new patients. They needed some scheduling flexibility, but they were not as overwhelmed as we initially thought.
That is when the MATTERS concept was born: we wanted to streamline the process of linking people with OUD to outpatient treatment. In partnership with UBMD Emergency Medicine—the physician group affiliated with the University of Buffalo— we onboarded one major hospital and three community-based treatment organizations as a pilot to demonstrate proof of concept. Each treatment organization chipped in weekly appointment availability so one single organization would not be overwhelmed. We have put the patient first and allowed them to choose which location they wanted to follow up at, which helped build autonomy and empowerment in their recovery journey.
How important is collaboration with other healthcare institutions locally for the treatment of addiction? What specific institutions have you found instrumental in treatment?
Collaboration has been vital for our program’s success. We know that our healthcare system is siloed, and instead of re-creating the wheel, we wanted to connect pre-existing resources to provide the best receiving network for patients. Local organizations are already committed to improving access to treatment for OUD because many of them know how pressing the issue is within their communities. Partnering with local organizations is also key because most patients want to receive treatment and support from someone familiar, not someone from across the state.
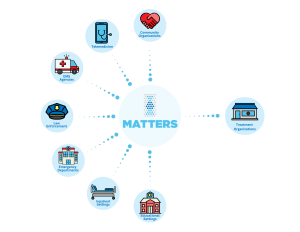
Without the support from the Jacobs School of Medicine and Biological Sciences at the University of Buffalo, as well as UBMD Emergency Medicine, our program would not be possible. Key stakeholders in expanding treatment include hospitals, insurance companies, law enforcement, EMS agencies, telemedicine agencies, EMS professionals, and peer organizations. Statewide institutions, such as the New York State Office of Addiction Services and Supports and the NYS AIDS Institute, have been instrumental in expanding the MATTERS program.
How is MATTERS presented/taught to other staff in your department?
MATTERS focuses on reframing how we think about addiction. We define OUD as a severe, life-threatening disease that typically requires treatment with medication. We try to use the term “medication for addiction treatment” rather than “medication-assisted treatment.” Why? Because for OUD, the medication is the treatment. It does the heavy lifting rather than assist in treating the condition.
When we present on the MATTERS program, we also focus on reducing the stigma associated with OUD. In medicine, we still refer to this disease as “abuse,” which can be stigmatizing and “othering” to patients. Abuse is such a negative, powerful word that carries a negative connotation. We draw attention to the fact that no one would choose to experience OUD, and OUD does not discriminate. When we address common barriers to treatment or meet a patient’s basic needs, they are much more likely to follow up for treatment. We also like to frame MATTERS as a one-stop solution for patients and providers alike. We built this program to be simple and effective for busy EM physicians trying to link patients to treatment.
What are common challenges encountered with MATTERS? How are they overcome?
Even with all of the support services we offer, it is difficult to consistently reach marginalized communities, specifically homeless populations—without a phone, email, or consistent transportation; it can be difficult to stay linked to care for this demographic. Another challenge is funding. Initially, we received several pilot grants to build MATTERS (from the Blue Cross Blue Fund along with the Oishei Foundation in Buffalo, NY). More recently as the program has grown, we have partnered with several New York State Agencies (primarily NYS Department of Health and OASAS) for support of the MATTERS program. We are evaluating options for federal funding to assist in the ability to offer MATTERS services to additional states.
We have overcome these challenges by improving access to our services. In the summer of 2022, we launched the MATTERS Network mobile app to place our resources directly at the fingertips of folks who need them most. We’ve also expanded to offer follow-up support services so that if someone is having a hard time staying linked to care, we can address those issues on an individual basis.
What advice can you offer to EM physicians interested in initiating a similar program to MATTERS but who have no background or training in this field? What are the first steps they can take to pursue this interest?
The first step is assessing the resources already available in your region. Recreating the wheel will always take longer and will be more complicated than building strategic partnerships with community-based organizations working toward the same goal as you. Use MATTERS as a resource! We’ve built this program with deliberate attention paid to the ability to replicate across the country in any emergency department (and beyond). We strive to serve as a national model for linkage to treatment for complex disease processes including, but not limited to, OUD, hepatitis, HIV, and mental health.
We’ve done a lot to build this program, and we want it to serve as a model for innovative treatment for OUD. Review our published research articles where we outline the development and results of the MATTERS program and other similar initiatives to better understand how you may start a similar program.



